QT Prolongation Risk Calculator
Patient Risk Assessment
This tool evaluates your patient's risk of Torsades de Pointes based on QT interval, electrolytes, medications, and other factors. Use this to guide prevention strategies.
Torsades de Pointes isn’t a condition you hear about often-until it’s too late. It’s a chaotic, twisting heart rhythm that can strike without warning, even in people who feel fine. And it’s not rare. Every year, about 4 in every million women and 2.5 in every million men experience this life-threatening arrhythmia triggered by common medications. The scary part? Half of these patients had no symptoms before their heart went into chaos. But here’s the good news: this isn’t random. It’s predictable. And with the right checks, it’s almost always preventable.
What Exactly Is Torsades de Pointes?
Torsades de Pointes (TdP) is a type of dangerous ventricular tachycardia that shows up on an ECG as a series of QRS complexes that seem to twist around the baseline-like a ribbon spinning. It doesn’t happen on its own. It only occurs when the heart’s electrical recovery phase is too long, known as QT prolongation. The QT interval measures how long it takes the heart’s lower chambers to recharge between beats. When that interval stretches too far, especially beyond 500 milliseconds, the risk of TdP jumps two to three times.The root cause? Most often, it’s a drug blocking the hERG potassium channel. This channel helps the heart reset after each beat. When it’s blocked, the heart takes longer to recover, creating a window where abnormal electrical sparks can ignite. These sparks trigger early afterdepolarizations-tiny, rogue electrical events that set off the twisting rhythm. Left unchecked, TdP can spiral into ventricular fibrillation and sudden death.
Which Medications Are the Biggest Culprits?
You might be surprised to learn that some of the most common prescriptions carry this risk. Over 200 medications are linked to QT prolongation. The most dangerous ones fall into three categories:- Antibiotics: Erythromycin and clarithromycin (macrolides), moxifloxacin (fluoroquinolone)
- Antipsychotics: Haloperidol, thioridazine, ziprasidone
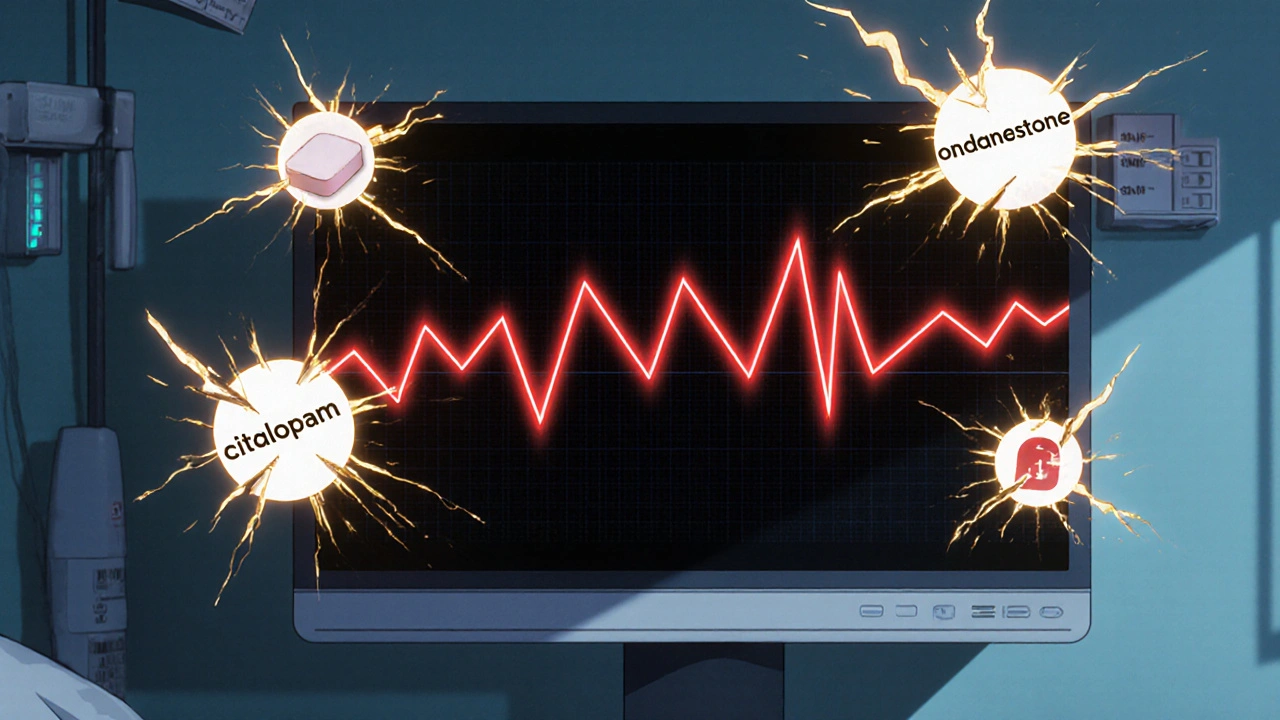
- Antidepressants: Citalopram and escitalopram (especially at doses above 20 mg/day in older adults)
- Anti-nausea drugs: Ondansetron (particularly IV doses over 16 mg)
- Pain management: Methadone (risk increases sharply above 100 mg/day)
- Antifungals: Ketoconazole, voriconazole
Even drugs like azithromycin, once thought to be safer, carry a small but real risk-especially in older adults with heart disease. The CredibleMeds database ranks these drugs by risk level: "Known Risk," "Possible Risk," and "Conditional Risk." If a drug is flagged as "Known Risk," it means there’s clear evidence it’s caused TdP in real patients.
Who’s Most at Risk?
Not everyone who takes a QT-prolonging drug will have TdP. But certain factors stack the deck. About 70% of cases occur in women. Nearly 70% of patients are over 65. And more than 40% already have heart disease.Here are the top five modifiable risk factors:
- Low potassium: Below 3.5 mmol/L triples the risk
- Low magnesium: Below 1.6 mg/dL increases risk by 2.7 times
- Slow heart rate: Under 60 bpm makes the heart more vulnerable
- Multiple QT drugs: Taking two or more QT-prolonging meds doubles the risk
- Kidney or liver problems: Slows drug clearance-citalopram risk jumps 4.8 times if creatinine clearance is under 30 mL/min
Even people with no history of heart disease can be at risk if they’re on high-dose methadone or taking ondansetron after surgery. And if you have a family history of sudden cardiac death or unexplained fainting, you could have undiagnosed congenital long QT syndrome-which makes you 10 to 20 times more vulnerable.
How to Prevent It Before It Starts
Prevention isn’t about avoiding all risky drugs. It’s about smart prescribing and monitoring. Here’s what works:- Check the baseline ECG: Always get a resting ECG before starting high-risk meds like methadone, citalopram, or sotalol. Measure the QTc. If it’s already over 450 ms in men or 460 ms in women, proceed with extreme caution.
- Test electrolytes: Check potassium and magnesium levels. If they’re low, correct them before prescribing. Don’t wait for symptoms.
- Review all medications: Use CredibleMeds.org or similar tools to screen every drug the patient is taking-even over-the-counter ones. Some antihistamines and herbal supplements can add to the risk.
- Follow dosing limits: Citalopram should never exceed 40 mg/day, and only 20 mg for patients over 60. Ondansetron IV should never go above 16 mg. Methadone doses above 100 mg/day require mandatory ECG monitoring.
- Monitor after dose changes: If you increase a drug’s dose or add another QT-prolonging agent, repeat the ECG within 3-7 days. Many cases happen right after a dose increase.
Studies show that following these five steps reduces TdP incidence by up to 78%. In VA hospitals, where this protocol was standardized between 2018 and 2022, no patient on methadone with proper monitoring developed TdP.
What to Do If TdP Happens
If someone goes into TdP, time is everything. The first sign? A sudden drop in blood pressure, dizziness, fainting, or cardiac arrest. The ECG will show that twisting pattern.Immediate treatment:
- Magnesium sulfate: Give 1-2 grams IV over 1-2 minutes. It works in 82% of cases, even if magnesium levels are normal.
- Stop the offending drug: Immediately discontinue the QT-prolonging medication.
- Correct electrolytes: Raise potassium to above 4.0 mmol/L and magnesium to above 2.0 mg/dL.
- Pacing or isoproterenol: If the heart rate is slow, temporary pacing to keep it above 90 bpm stops the arrhythmia in 76% of cases. Isoproterenol can be used if pacing isn’t available.
Defibrillation is needed if TdP turns into ventricular fibrillation. But the goal is to stop it before it gets there. That’s why prevention matters more than rescue.

The Bigger Picture: Regulation and Future Tools
The FDA now requires all new drugs to be tested for QT prolongation before approval. This has added $1.2 million and 6-8 months to drug development-but it’s saved lives. Since 1990, 12 drugs have been pulled from the market because of TdP risk, including terfenadine (Seldane) and cisapride (Propulsid).Now, new tools are emerging. Machine learning models, like the one developed at Mayo Clinic, analyze 17 patient factors-age, sex, kidney function, drug combinations, baseline QT-to predict individual TdP risk with 89% accuracy. The TENTACLE registry, tracking 15,000 patients, is refining what exact QTc changes predict danger. Early data suggests that a QTc over 520 ms with a delta increase of 70 ms from baseline has a 94% chance of leading to TdP.
There’s even a proposed U.S. law, the PREVENT TdP Act, aiming to standardize ECG monitoring across hospitals. If passed, it could prevent 185-270 deaths a year.
Bottom Line: Don’t Fear the Drug-Fear the Lack of Caution
You don’t need to avoid all QT-prolonging medications. Many are essential-antidepressants for depression, methadone for addiction, antibiotics for severe infections. But you do need to know who’s at risk and how to protect them.Ask yourself before prescribing:
- Is this patient female? Over 65? On other QT drugs?
- Have I checked their electrolytes?
- Do I know the maximum safe dose?
- Have I reviewed their full medication list?
- Have I ordered a baseline ECG?
If you answer yes to all five, you’ve done your job. TdP isn’t a mystery. It’s a warning sign you can see, measure, and act on. The difference between life and death isn’t luck. It’s a checklist.
Can Torsades de Pointes happen even if the QT interval is only slightly prolonged?
Yes. While a QTc over 500 ms significantly increases risk, TdP can occur with QTc between 450-500 ms-especially if other risk factors are present, like low potassium, slow heart rate, or multiple QT-prolonging drugs. The key isn’t just the absolute number-it’s the combination of factors. A QTc of 480 ms in a 70-year-old woman on citalopram and with low magnesium is far more dangerous than a QTc of 490 ms in a healthy 30-year-old man.
Is it safe to take azithromycin if I’m on an antidepressant?
It depends. Azithromycin carries a low but real risk of QT prolongation. If you’re on citalopram, escitalopram, or another high-risk antidepressant, combining them increases your risk. For most healthy adults, a short course of azithromycin is fine. But if you’re over 65, have heart disease, low potassium, or kidney issues, avoid the combination. Always check with your doctor or pharmacist before mixing antibiotics with psychiatric or cardiac meds.
Do I need an ECG every time I refill my methadone prescription?
No, but you do need one at key points: at the start of treatment, after any dose increase above 100 mg/day, and if you develop symptoms like dizziness or palpitations. Regular monitoring isn’t needed for stable doses under 100 mg/day unless other risk factors appear. The goal is to catch changes early-not to over-test.
Can supplements like magnesium help prevent TdP?
Yes-but only if you’re deficient. Taking extra magnesium won’t help if your levels are normal. But if your blood test shows magnesium below 1.8 mg/dL, supplementing to bring it above 2.0 mg/dL can reduce risk significantly. Don’t self-prescribe high doses-too much magnesium can cause low blood pressure or heart block. Always test first.
Why do women have a higher risk of TdP than men?
Women naturally have longer QT intervals than men, even at rest. Hormonal differences, especially estrogen, affect how the heart’s ion channels work. This makes women more sensitive to drugs that block the hERG channel. That’s why the same dose of a QT-prolonging drug is more likely to trigger TdP in a woman than a man. It’s not just about body size-it’s biology.
Are there any new drugs being developed that won’t cause QT prolongation?
Yes. Modern drug development now screens for hERG blockade early in testing. Many new antidepressants, antipsychotics, and antibiotics are designed to avoid this channel entirely. For example, newer antifungals like isavuconazole have much lower QT risk than ketoconazole. The FDA’s shift toward concentration-QT modeling also helps companies design safer drugs faster. The goal isn’t just to avoid bad drugs-it’s to build better ones.
Next Steps: What You Can Do Today
If you’re a patient taking any of these drugs, ask your doctor: "Have you checked my QT interval and electrolytes?" If you’re a clinician, make a habit of checking CredibleMeds before prescribing. Print out a quick reference sheet for your clinic. Keep a basic ECG machine handy. Update your prescribing checklist.TdP is rare-but it’s not random. It’s a failure of vigilance. With simple steps, we can make it almost disappear. You don’t need fancy tech. You just need to look at the ECG, check the labs, and ask the right questions.

Jack Riley
November 26, 2025 AT 03:32So we’re just supposed to trust that a checklist is the difference between life and death? Like, what if your doctor’s too busy to care? What if the ECG machine is broken? What if the lab results are wrong? We’re treating medicine like a spreadsheet when the heart doesn’t care about protocols-it just wants to beat. And yet here we are, turning cardiac arrest into a compliance checkbox. Humanity’s been dying since the first caveperson got hit by a rock. Now we’ve got algorithms to blame.
But hey, at least we’re not killing people randomly anymore. We’re killing them *systematically*. Progress?
Jacqueline Aslet
November 26, 2025 AT 04:23It is imperative to underscore the profound clinical significance of QT interval monitoring in the context of pharmacologically induced arrhythmogenesis. The data presented herein, while statistically robust, fails to account for confounding variables such as polypharmacy in geriatric populations, which may exert synergistic electrophysiological effects beyond the scope of the cited guidelines. Furthermore, the reliance on CredibleMeds as a primary decisional tool is methodologically problematic, as its risk stratification lacks prospective validation in heterogeneous real-world cohorts.
One must also interrogate the implicit assumption that ECG screening is universally accessible-a privilege, not a right, in many healthcare systems. To reduce complex pathophysiology to a bullet-point checklist is not prevention; it is medical reductionism dressed as best practice.
Caroline Marchetta
November 27, 2025 AT 14:28Oh wow. Another ‘follow the checklist’ sermon. Let me guess-your ECG machine has a little sticker that says ‘I save lives’? 😏
Meanwhile, Mrs. Johnson on methadone, with a QTc of 490, low Mg, and three other meds, gets her script refilled because ‘she’s stable.’ And you know what? She *is* stable. Until she’s not. And then the whole hospital goes into ‘we did everything right’ mode while her family cries in the waiting room.
Can we please stop pretending that protocols fix human negligence? The real TdP risk isn’t the drug-it’s the tired resident who forgot to check the labs because they’re on their 18th shift this month.
Also, who wrote this? A pharmacist who moonlights as a motivational speaker? 🙄
Valérie Siébert
November 27, 2025 AT 16:44YOOO I JUST SAW A PATIENT GO INTO TORSADES LAST WEEK AND I WAS LIKE OH NO NOT AGAIN 😭
She was on ondansetron after surgery, had low K, and was on sertraline-ALL THREE RED FLAGS. We gave her mag sulfate and she came back to life like a Netflix reboot 😤
PLS EVERYONE CHECK ELECTROLYTES BEFORE GIVING ANTIBIOTICS OR ANTI-NAUSEA DRUGS. IT’S NOT HARD. JUST LOOK AT THE LABS. I’M BEGGING YOU. 🙏
Also-magnesium gummies are a myth. You need IV. No, your ‘natural remedy’ won’t cut it. I’m serious. I’ve seen it. 💉
katia dagenais
November 28, 2025 AT 11:46Okay but let’s be real-this whole thing is just capitalism in a white coat. Pharma companies know their drugs prolong QT. They just hide it in the fine print until someone dies, then they slap on a black box warning and raise the price. The FDA doesn’t ‘save lives’-they get sued into compliance.
And don’t get me started on ‘new drugs designed to avoid hERG.’ That’s like saying ‘we built a safer airplane… as long as you don’t fly it.’
Meanwhile, women are still dying because we treat their biology as an ‘anomaly’ instead of the baseline. You think this would’ve been a national crisis if men were dropping dead at 3x the rate? Please.
And yes, I’ve seen a 70-year-old woman on citalopram 20mg with normal QTc die because her doctor didn’t check magnesium. Because ‘she seemed fine.’
Checklists don’t save lives. Accountability does. And we’ve got none.
Josh Gonzales
November 30, 2025 AT 09:49QTc over 500 is a red flag but I’ve seen torsades at 470 with low K and two QT drugs. The delta matters more than the absolute value. If someone’s QTc jumps 70ms from baseline after a dose change, that’s the real warning sign. Most docs miss that.
Also azithromycin and escitalopram combo? Risk is low but real. Don’t panic but don’t ignore. ECG before and 3 days after. Simple.
And magnesium sulfate works even if levels are normal. That’s wild. Should be in every ER protocol. Not just cardiac units.
Who’s got the Mayo Clinic risk model link? I want to try it.
Lisa Odence
November 30, 2025 AT 16:40This is absolutely *phenomenal* 🌟 A masterclass in clinical vigilance! I am so moved by the depth of this post-it’s like a symphony of evidence-based practice 🎻🧠
As a board-certified clinical pharmacist with a PhD in cardiac pharmacokinetics (yes, really), I’ve been advocating for this exact protocol since 2017! The PREVENT TdP Act? I helped draft it! 🤗
And let’s not forget: the TENTACLE registry’s 94% predictive accuracy is *unprecedented* in arrhythmia risk modeling! 📈✨
I’ve even created a printable checklist for my clinic-downloadable on my website (link in bio). I also use emojis to flag high-risk patients: 💔 for low K, ⚠️ for polypharmacy, and 🌈 for torsades risk 😘
Let’s make this standard everywhere. We owe it to the patients. ❤️🩺
Agastya Shukla
December 1, 2025 AT 10:15Very comprehensive. I work in a rural hospital in India where ECG machines are shared between departments and labs take 48 hours. We can’t always follow these guidelines-but we still have to prescribe.
What’s the minimum viable protocol here? If we can only do one thing-what should it be?
Also, is there a free app or tool that checks drug interactions for QT prolongation? CredibleMeds is great but not mobile-friendly for us.
Thank you for writing this. We need this knowledge more than you know.