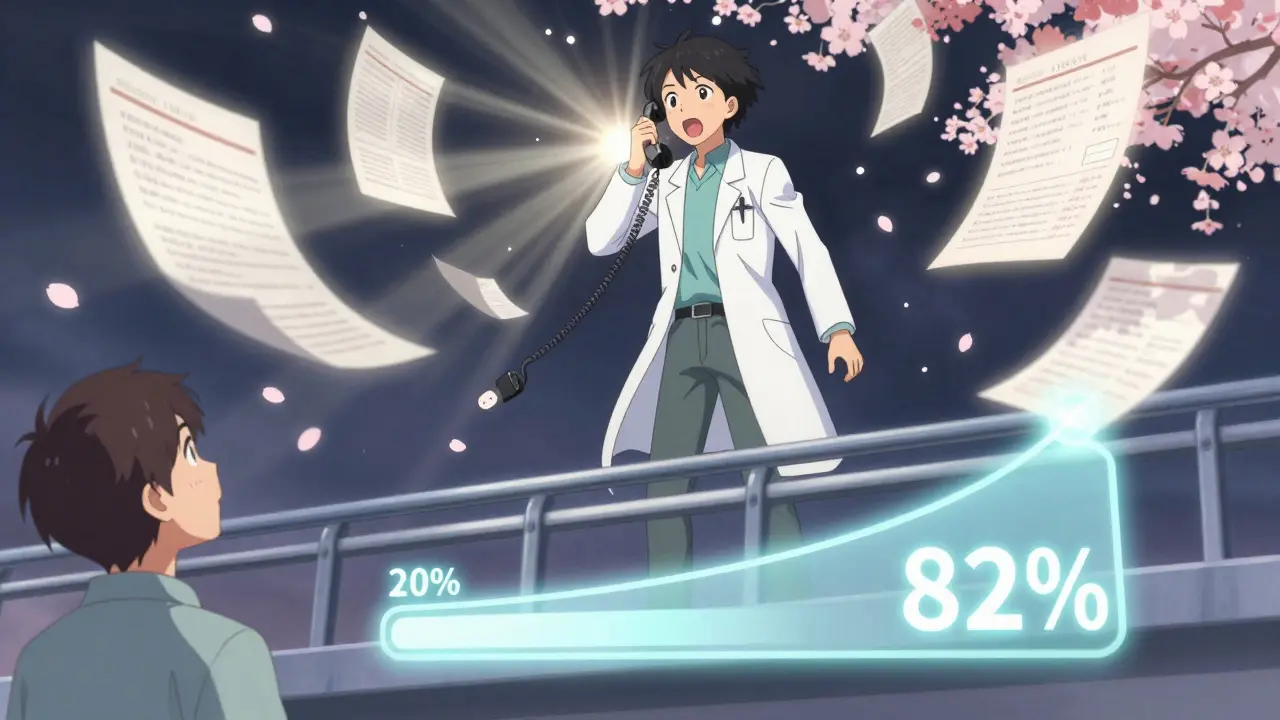
If your insurance denied coverage for a medication your doctor prescribed, you’re not alone. About 6% of prior authorization requests get turned down - but here’s the thing: 82% of those denials get reversed when you appeal. That means most people who give up are losing access to medicine they need - not because the drug isn’t right for them, but because the paperwork got messed up.
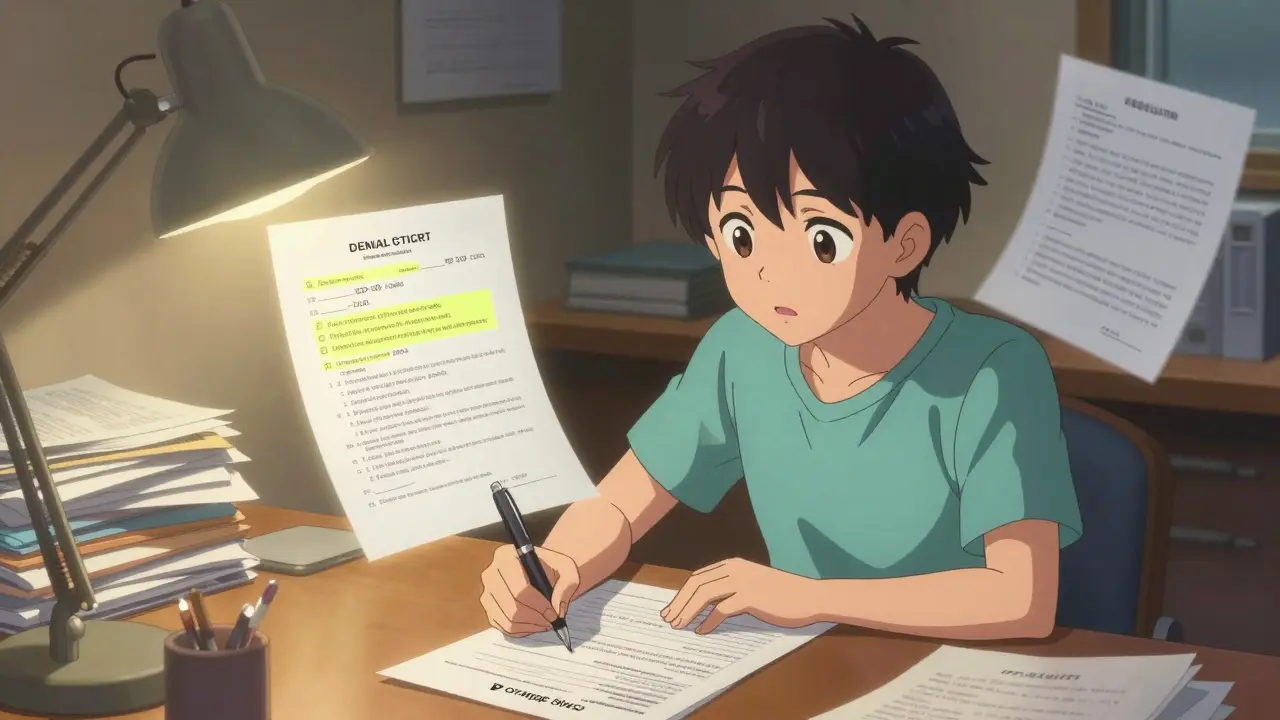
Understand Why Your Medication Was Denied
The first step isn’t to panic or call your doctor right away. It’s to read the denial letter. Seriously. Most people skim it or toss it. But that letter tells you exactly why you were denied. There are three main reasons:- Incomplete paperwork (37% of denials): Missing forms, wrong ID numbers, or a signature that’s smudged.
- Lack of medical necessity (48%): The insurer says your condition doesn’t meet their criteria for this drug - even if your doctor disagrees.
- Not covered by your plan (15%): The drug isn’t on their formulary, or you didn’t try cheaper alternatives first.
Gather Everything Your Doctor Needs to Support You
You can’t appeal with just a letter from your doctor saying “please cover this.” You need evidence. Here’s what works:- Full medical records showing your diagnosis and treatment history
- Lab results, imaging reports, or test outcomes that prove your condition
- Notes from your doctor explaining why this specific drug is necessary - not a generic one
- A list of other medications you’ve tried, with dates and outcomes (e.g., “Metformin, 6 months, no improvement in HbA1c”)
- Any documentation of side effects or allergic reactions to alternatives
Follow Your Insurer’s Exact Appeal Process
Every insurance company has its own rules. You can’t just email a letter and hope for the best. Here’s how to do it right:- Find your plan’s appeal form. It’s usually on their website under “Member Services” or “Prior Authorization.”
- Some, like CVS/Caremark, require faxing documents to a specific number (1-888-836-0730). Others, like UnitedHealthcare, require online portal submissions.
- Make sure your appeal includes: your full name, member ID, date of birth, drug name, and your doctor’s contact info.
- Submit within 180 days of the denial. This is federal law under the Affordable Care Act.
Write a Clear, Evidence-Based Appeal Letter
Your letter isn’t a plea. It’s a clinical argument. Use this structure:- State the purpose: “I am formally appealing the denial of [Drug Name] for [Condition].”
- Address the denial reason: If they said “lack of medical necessity,” quote their own criteria from the plan document and show how your case meets it.
- Include clinical evidence: “Patient has tried three first-line agents: [List drugs, doses, durations, outcomes]. All resulted in [side effects / no improvement].”
- Reference codes: Include the ICD-10 diagnosis code and CPT code for the medication. 89% of approved appeals include these.
- End with a request: “Please approve coverage immediately to prevent worsening of condition.”
Get Your Doctor Involved
Your doctor doesn’t just sign a form. They need to call the insurer directly. Many insurers have a “peer-to-peer review” option - where your doctor talks to a medical director from the insurance company. This step alone increases approval odds by 32%. Ask your doctor’s office to:- Call the number on the denial letter and ask for “clinical review” or “peer-to-peer”
- Have your full chart ready during the call
- Document the date, time, name of the reviewer, and what was discussed
Track Every Step and Follow Up
Insurers say they’ll respond in 30 days. But 78% of physicians report having to call multiple times. Don’t wait. Keep a log:- Date you submitted the appeal
- Who you spoke to (name, ID, date)
- What they promised
- Any reference numbers
What If Your Appeal Gets Denied Again?
You have one more step: an external review. This is when an independent third party - not your insurer - looks at your case.- You have 365 days from the final denial to request this (federal rule).
- Some states have shorter windows - check your state’s insurance department website.
- You can request this even if you didn’t appeal internally - but it’s better to do both.
Common Mistakes That Kill Appeals
People lose appeals for simple reasons:- Not including CPT or ICD-10 codes
- Using vague language like “my doctor says this is needed” instead of clinical evidence
- Missing deadlines - especially for external reviews
- Not following the insurer’s submission method (fax vs. portal vs. mail)
- Not keeping copies of everything
How Long Does This Take?
It’s not fast. But it’s worth it.- Initial appeal: 14-30 days
- External review: 30-60 days
- Time spent: 6-8 hours total per appeal
What If You Can’t Afford the Medication While You Wait?
Some drug manufacturers offer patient assistance programs. Ask your pharmacist or search the manufacturer’s website. Organizations like NeedyMeds and Patient Access Network Foundation can help with co-pays. Your doctor might also have samples or coupons. Don’t assume you’re out of options until you’ve asked.There’s no magic trick. But there is a proven system. Know the reason for the denial. Gather the evidence. Follow the rules. Get your doctor on the line. Track everything. And don’t quit.
Medication isn’t optional. Your health isn’t a line item on an insurance spreadsheet. If you’ve been denied, you have rights - and the system, flawed as it is, is designed to let you fight back. Use them.
What should I do if my insurance denies my medication without giving a reason?
Insurers are legally required to explain why they denied coverage. If you received a denial letter with no clear reason, call them immediately and ask for a formal explanation in writing. If they refuse, file a complaint with your state’s insurance department. You can also request an external review, which forces an independent review of your case.
Can I appeal if I’m on Medicare Advantage?
Yes. Medicare Advantage plans must follow federal appeal rules, and they have a higher success rate than commercial insurers - about 22% higher. You have 60 days to appeal internally, then 365 days to request an external review. CMS now requires these plans to respond to prior authorization requests within 72 hours, which reduces the need for appeals in many cases.
How long do I have to file an appeal?
You have 180 days from the date of the denial letter to file an internal appeal. For an external review, you have 365 days. Some states have shorter deadlines for external reviews - check your state’s insurance commissioner website. Never assume you have more time than what’s written in your denial letter.
Do I need a lawyer to appeal a prior authorization denial?
No. Most people successfully appeal without legal help. The key is following the insurer’s process exactly and submitting strong clinical evidence. Lawyers are only necessary if you’re dealing with a complex ERISA plan or if you’ve exhausted all other options and still face denial. Patient advocacy groups can help for free.
Why do insurers deny medications even when my doctor says they’re necessary?
Insurers use clinical guidelines and cost controls to decide what to cover. Sometimes, their rules are outdated or don’t match real-world treatment needs. A 2023 AMA survey found that 41% of denials were due to administrative errors - not medical reasons. That’s why detailed appeals with specific data - like treatment failures or lab results - reverse denials 82% of the time.
What if my doctor won’t help me appeal?
Your doctor has a legal and ethical duty to support your care. If they refuse, ask why. If it’s because they’re too busy, ask for a referral to another provider or a nurse practitioner who can help. You can also request a written statement from them explaining their position - even if it’s negative, it can help your appeal. If you feel your doctor is abandoning you, contact your state medical board.




Meghan O'Shaughnessy
December 18, 2025 AT 04:38Just got my insulin appeal approved after 3 tries. The key? Sending the lab results with the exact dates and the doctor’s handwritten note on top. They can’t ignore that.
Also, always send it certified mail. Paper trail saves lives.
Kaylee Esdale
December 19, 2025 AT 23:09Been there. Lost my meds for 4 months. Then I printed every single note from my neurologist, stapled it like a book, and mailed it with a post-it that said ‘This isn’t optional. I need this to walk.’ They approved it in 11 days.
Stop begging. Start presenting.
Jody Patrick
December 21, 2025 AT 10:45Insurance is just corporate greed wrapped in bureaucracy. No wonder people die waiting. Fix the system, not your appeal letter.
Radhika M
December 22, 2025 AT 16:28My sister in Mumbai got her cancer drug approved using this exact method. The CPT code was the magic key. Always include it. No excuses.
Philippa Skiadopoulou
December 24, 2025 AT 01:10While the procedural advice is sound, one must acknowledge that systemic inefficiencies in prior authorization reflect broader failures in healthcare financing. The burden placed on patients is disproportionate and ethically questionable.
Nonetheless, adherence to protocol remains the most viable path forward under current constraints.
Pawan Chaudhary
December 24, 2025 AT 13:51You got this! I know it feels overwhelming but you’re not alone. I appealed for my dad’s heart med and we won. Keep going. One step at a time. 💪
CAROL MUTISO
December 26, 2025 AT 06:21Wow. So we’re supposed to become medical record archivists now? Because apparently, in 2024, getting a life-saving drug requires a PhD in insurance legalese.
Let me guess-next they’ll make us file appeals in triplicate while reciting the Affordable Care Act backwards.
At least my doctor doesn’t have to do this. No wonder they’re burned out.
Meanwhile, the CEO of my insurer just bought a third yacht.
But hey, at least we have ‘clinical evidence’ now. What a world.
Erik J
December 27, 2025 AT 00:49Interesting stats. But I wonder-how many of those 82% reversals were due to actual medical necessity versus administrative errors being corrected? Is the system just broken, or are we optimizing around a broken design?
BETH VON KAUFFMANN
December 28, 2025 AT 14:19Let’s be real-most of these appeals fail because patients don’t understand ICD-10 coding hierarchies or the difference between CPT 99213 and 99214. If you can’t articulate the clinical justification using CMS guidelines, you’re just noise.
And don’t even get me started on the 180-day window-most people miss it because they don’t know ERISA preempts state law in group plans.
TL;DR: If you didn’t read the Blue Cross Provider Manual, you’re not qualified to appeal.
Martin Spedding
December 29, 2025 AT 00:38LOL. You think this works? My friend sent a 47-page dossier with bloodwork and a PowerPoint. Got denied again. Then he called the CEO’s assistant. Got approved next day.
Turns out, screaming into the void works better than evidence.
Also, typo on page 32. I saw it. You’re doomed.
Raven C
December 30, 2025 AT 10:25How utterly... pedestrian. To reduce the sanctity of therapeutic autonomy to a bureaucratic checklist is to misunderstand the very essence of medical ethics.
One does not ‘appeal’ for dignity. One demands it.
And yet, here we are-reduced to submitting forms like serfs petitioning the lord for grain.
Perhaps we should all just move to Canada. Or die quietly.
Patrick A. Ck. Trip
January 1, 2026 AT 07:06Thank you for this comprehensive guide. I am deeply moved by the resilience of individuals navigating such a flawed system.
While I recognize the emotional toll, I believe that patience, meticulous documentation, and unwavering hope are virtues that ultimately prevail.
May you find strength in the process, and may your health be restored with grace and dignity.
Chris Van Horn
January 3, 2026 AT 06:56Pathetic. You people actually think paperwork fixes this? The system is rigged. The insurers know you’ll quit. They count on it. And you’re still following their stupid 180-day rule like it’s holy scripture?
Go to the state AG’s office. File a class-action. Or just show up at their HQ with a sign.
Appeals are a scam. Don’t play their game.
amanda s
January 3, 2026 AT 22:17My husband died waiting for his lung med to be approved. They said ‘lack of medical necessity.’ He was on oxygen. They didn’t even call his doctor.
So yeah. Do your paperwork. But also? Burn it all down.
Brooks Beveridge
January 5, 2026 AT 14:19You got this, warrior. 🙌
Every form you fill, every call you make-it’s not just for you. It’s for everyone who comes after you.
And if your doctor won’t help? Find one who will. You’re not a patient. You’re a patient advocate now.
Keep going. I believe in you.