Medication Timing Calculator for Bladder Control
How Medication Timing Affects Your Bladder
Many common medications can cause frequent urination or urgency. Timing your dose can significantly reduce nighttime trips to the bathroom. Based on clinical evidence, this tool helps you find the optimal time to take your medication.
Waking up three times a night to use the bathroom? Feeling a sudden, intense urge to go even when your bladder isn’t full? You might blame aging, coffee, or stress-but what if it’s your medication? Many people don’t realize that common prescriptions can directly trigger bladder problems, and the fix isn’t always stopping the drug-it’s adjusting how and when you take it.
Why Your Medication Is Making You Pee More
Your bladder doesn’t work in isolation. It’s controlled by nerves, muscles, and hormones that can be disrupted by drugs meant for other parts of your body. Medications that cause frequent urination or urgency don’t just make you produce more urine-they interfere with how your bladder stores or empties it. The result? You feel the need to go often, even if you just went, or you can’t hold it when the urge hits. The most common offenders fall into a few key groups. Diuretics, calcium channel blockers, antidepressants, and anticholinergics are the top culprits. According to the International Continence Society, at least 12 major classes of medications are linked to lower urinary tract symptoms. And it’s not rare: up to 20% of adults over 40 with frequent urination have it tied to their meds, not aging or prostate issues.Diuretics: The Big One
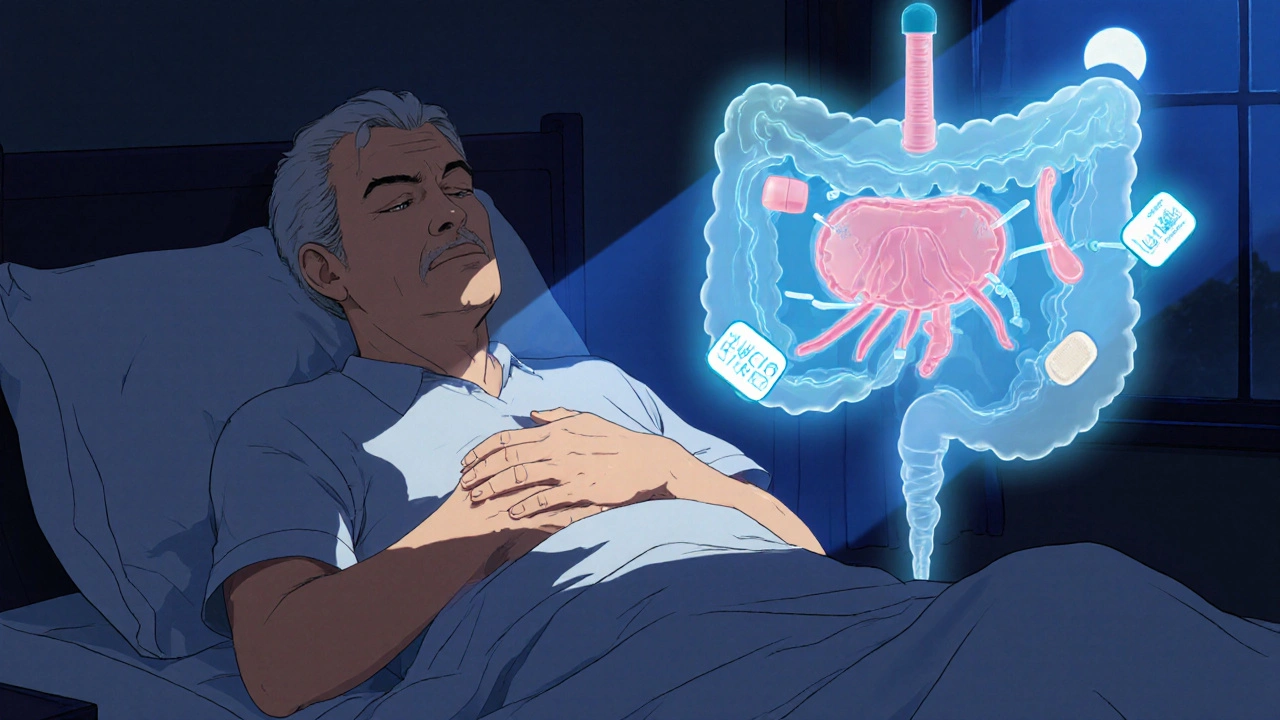
If you’re on a water pill-like hydrochlorothiazide, furosemide (Lasix), or spironolactone (Aldactone)-you’re in the majority. These drugs are prescribed for high blood pressure, heart failure, or swelling, and they work by making your kidneys flush out extra salt and water. That’s good for your heart, but hard on your bladder. Within two hours of taking a diuretic, urine output can jump by 20-50%. That means your bladder stretches more than usual, and your brain gets the signal: empty now. About 65% of people on diuretics report peeing more during the day, and 40% wake up at night to go. The higher the dose, the worse it gets. One study found that 28% of people taking 80mg of furosemide daily needed incontinence products because of sudden urges, compared to just 8% on 20-40mg. The fix? Timing. Taking your diuretic before 2 p.m. cuts nighttime bathroom trips by 60%. No more 2 a.m. wake-ups. Splitting the dose-say, half in the morning and half at lunch-can also help. One patient on Healthgrades reported dropping from 12 daily bathroom visits to just 5 after switching from a single morning dose to two smaller ones.Calcium Channel Blockers: The Silent Bladder Saboteur
If you’re on amlodipine, nifedipine, or verapamil for high blood pressure, your bladder might be paying the price. These drugs relax blood vessels to lower pressure, but they also relax the detrusor muscle in your bladder wall. That muscle needs to contract to push urine out. When it’s sluggish, your bladder doesn’t empty well, which leads to overfilling and then sudden, strong urges. A 2019 meta-analysis showed people on nifedipine averaged 1.8 more nighttime bathroom trips than those on placebo. Verapamil had the highest risk-42% of users reported significant nocturia. Symptoms usually show up within 2-4 weeks of starting the drug. Unlike diuretics, this isn’t about volume-it’s about control. Your bladder feels full even when it’s not, and you can’t ignore it.
Antidepressants and Mood Stabilizers: When Your Mind Affects Your Bladder
Antidepressants like venlafaxine (Effexor), escitalopram (Lexapro), and fluoxetine (Prozac) are linked to overactive bladder in 22% of users. These drugs change serotonin and norepinephrine levels, which directly influence bladder nerve signaling. The result? A bladder that contracts too easily or too often. Lithium, used for bipolar disorder, has a different but equally disruptive effect. About 1% of long-term users develop nephrogenic diabetes insipidus. This means the kidneys can’t concentrate urine, so you produce 3+ liters a day-sometimes even 5. That’s not just frequent urination; it’s constant, exhausting output. Nine percent of patients in one study stopped lithium because of urinary side effects. Antipsychotics like clozapine, risperidone, and olanzapine also cause issues. They block acetylcholine, a chemical needed for bladder contraction. This can lead to incomplete emptying, which feels like urgency and increases infection risk.Other Surprising Culprits
You might not think of allergy meds, but antihistamines like diphenhydramine (Benadryl) can relax the bladder too much. Instead of urgency, you get retention-your bladder fills but doesn’t empty. That leads to overflow incontinence: you leak because it’s too full. About 5-7% of users experience this. ACE inhibitors like captopril can cause a dry cough, and that cough puts pressure on the pelvic floor. That’s stress incontinence-leaking when you sneeze, laugh, or lift something. About 15% of captopril users report this. Alpha-blockers like tamsulosin (Flomax) are prescribed for enlarged prostates to help with urination. They work by relaxing the prostate and bladder neck. But in 25-30% of men, they cause retrograde ejaculation-semen goes backward into the bladder instead of out. It’s not harmful, but it’s startling and affects sexual health.
What to Do If Your Meds Are Causing Problems
Don’t stop your medication on your own. But do talk to your doctor. Start by asking: Could this be the drug? If your symptoms started within the last 4-6 weeks, that’s a strong clue. Your doctor should follow a simple 4-step approach:- Confirm timing-did symptoms begin after starting the drug?
- Rule out other causes with a urine test and post-void residual check (to see if you’re emptying fully).
- Try non-drug fixes first: timing adjustments, bladder training, pelvic floor exercises.
- If symptoms persist, consider lowering the dose or switching to a different drug with fewer bladder effects.

Erika Sta. Maria
November 21, 2025 AT 15:00Steve Harris
November 22, 2025 AT 12:21Logan Romine
November 24, 2025 AT 05:32Chris Vere
November 25, 2025 AT 19:05Pravin Manani
November 26, 2025 AT 22:27Mark Kahn
November 28, 2025 AT 07:32Leo Tamisch
November 28, 2025 AT 15:33Daisy L
November 29, 2025 AT 21:09Anne Nylander
November 30, 2025 AT 08:39