When you pick up a prescription at the pharmacy, you might see two different names on the bottle: one that sounds familiar, like Lyrica, and another that’s shorter and cheaper, like pregabalin. You might wonder - is this generic version really the same? The answer lies in a term you’ve probably never heard before: bioequivalent.
What bioequivalence actually means
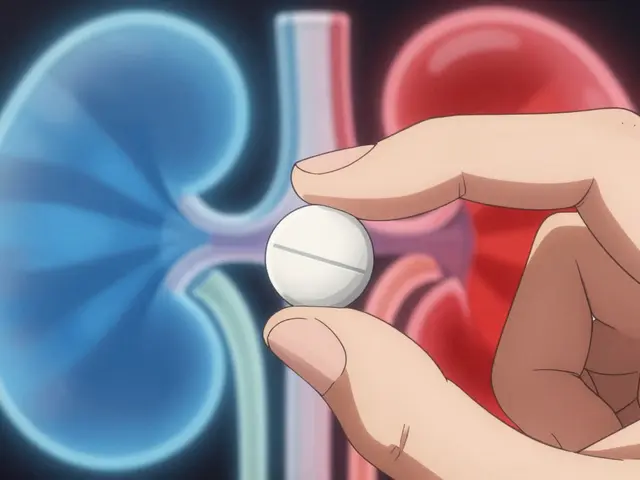
Bioequivalence isn’t about chemicals being identical. It’s about performance. Two drugs are bioequivalent if they deliver the same amount of active ingredient into your bloodstream at roughly the same speed. That’s it. No magic. No hidden differences. Just science. The U.S. Food and Drug Administration (FDA) defines it clearly: if two drugs have the same active ingredient, and when taken under the same conditions, they produce nearly identical levels in your blood over time, they’re bioequivalent. The standard? The amount of drug absorbed (measured as AUC) and how fast it gets there (measured as Cmax and tmax) must fall within 80% to 125% of the brand-name version. That’s not a random number. It’s based on decades of data showing that a 20% difference in absorption doesn’t change how the drug works in your body - for most medications. This isn’t theoretical. Over 90% of all prescriptions filled in the U.S. are for generic drugs. And if they weren’t bioequivalent, we’d be seeing massive spikes in treatment failures, hospitalizations, or side effects. We’re not. The system works.How bioequivalence is tested
You can’t just compare pill ingredients under a microscope. Two drugs might look the same, but if one dissolves slower or gets absorbed differently in the gut, it won’t work the same. That’s why testing happens in people - healthy volunteers, usually between 24 and 36 of them. Here’s how it works: participants take the brand-name drug one day, then the generic version a week later (or vice versa), after fasting. Blood samples are drawn over 24 to 72 hours. Scientists plot how much drug shows up in the blood over time. The area under that curve (AUC) tells them total exposure. The peak concentration (Cmax) and when it hits (tmax) tell them how fast it gets there. If the 90% confidence interval for both AUC and Cmax falls between 80% and 125% compared to the brand, the generic is approved. For most drugs, that’s enough. But for drugs where even a tiny change can be dangerous - like seizure meds or blood thinners - the FDA tightens the rules. For those, the range narrows to 90% to 111%. That’s called a narrow therapeutic index, and it’s why some doctors are extra cautious with these.Pharmaceutical equivalence vs. therapeutic equivalence
Don’t confuse bioequivalence with pharmaceutical equivalence. Pharmaceutical means the pills contain the same active ingredient, in the same strength, same form (tablet, capsule, etc.), and meet the same quality standards. But they can have different fillers, dyes, or coatings. That’s fine - as long as those differences don’t change how the drug behaves in your body. Therapeutic equivalence is the real goal. It’s when two drugs are both pharmaceutical equivalents AND bioequivalent. The FDA calls these “A-rated” drugs and assigns them an “AB” code in the Orange Book - the official list of approved generics. If a drug is AB-rated, pharmacists can substitute it without asking your doctor. That’s the whole point of the system: safe, affordable swaps.
Why some people feel the difference
If the science says they’re the same, why do some patients swear their generic doesn’t work as well? It’s real - and it happens. A 2021 study in JAMA Internal Medicine found that 0.8% of people switching from brand to generic antiepileptic drugs had breakthrough seizures. That’s rare, but it’s not zero. The most common culprits? Drugs with narrow therapeutic windows. Levothyroxine, for example, is used to treat hypothyroidism. Even a small change in absorption can throw hormone levels off. That’s why many doctors and pharmacists recommend sticking with the same generic manufacturer once you’ve stabilized. Some states even require pharmacies to notify you if they switch brands. But here’s the bigger picture: a 2022 survey of over 1,200 independent pharmacists found 87% reported no noticeable differences between brand and generic meds for most conditions. Consumer Reports’ 2023 survey of 3,421 people showed 78% were satisfied with generics - only 4 percentage points below brand-name users. And the FDA’s adverse event database shows generic-related complaints make up just 0.3% of all reports - proportional to their market share. So yes, some people notice a difference. But for the vast majority? It’s noise, not a signal.What’s behind the cost difference
A generic drug can cost 80% less than the brand. How? Because the generic maker doesn’t have to repeat expensive clinical trials. They only need to prove bioequivalence. The average cost to develop a generic? Around $2.2 million - and about a third of that goes to bioequivalence studies. Compare that to the $2 billion+ it takes to bring a new brand-name drug to market. The savings add up. Over the past decade, generics have saved the U.S. healthcare system an estimated $2.2 trillion. On average, each prescription saves patients $313. That’s not a small thing - especially for people on fixed incomes or managing chronic conditions.



dean du plessis
December 28, 2025 AT 14:30Interesting read. I've been on generics for years and never had an issue. My blood pressure meds work just as well as the brand, and I save like $100 a month. No drama, just science.
Janice Holmes
December 30, 2025 AT 13:24Let me tell you - I switched from Lyrica to pregabalin and my anxiety went from ‘manageable’ to ‘I need to call 911.’ The FDA’s 80-125% range? That’s not science - that’s corporate math. My body didn’t get the memo.
Liz Tanner
December 31, 2025 AT 23:14Janice, I hear you. I had a similar experience with levothyroxine - switched generics and my TSH went nuts. It’s not ‘all in your head.’ Sometimes the fillers or coating change how it dissolves. Talk to your pharmacist about sticking with the same manufacturer.
Gerald Tardif
January 1, 2026 AT 03:37Generics saved my life. I’m on three meds for chronic conditions. Without generics, I’d be choosing between insulin and rent. The system ain’t perfect, but it’s the best thing we’ve got. Don’t let a few bad stories scare you off the 97% who do just fine.
Babe Addict
January 1, 2026 AT 10:37Oh please. The FDA’s ‘bioequivalence’ is a joke. They test on 24 healthy young men who don’t even have the condition. What about elderly patients with kidney issues? Or people on multiple drugs? The whole system is rigged to favor Big Pharma’s profit margins.
John Barron
January 2, 2026 AT 17:33😂 I love how people think ‘bioequivalence’ means ‘identical.’ It’s like saying two BMWs are the same because they both have four wheels. The fillers, the coating, the dissolution rate - those matter. My uncle had a seizure after switching generics. He’s fine now, but… 😔
Kishor Raibole
January 3, 2026 AT 19:59It is not merely a matter of pharmacokinetic parameters; it is a metaphysical question of identity. When one ingests a substance, is it the same entity if the excipients differ? The soul of the medication - if one may be so bold - resides not only in the molecule but in its context. The FDA, in its bureaucratic wisdom, reduces the human body to a test tube.
Satyakki Bhattacharjee
January 5, 2026 AT 16:37Western medicine is a lie. In India, we use Ayurveda. One herb, one truth. No labs, no percentages. Your body knows what it needs. You are poisoned by science.
Will Neitzer
January 6, 2026 AT 13:12As a clinical pharmacist with 22 years in practice, I can confirm: bioequivalence standards are among the most rigorously enforced in pharmaceutical regulation. The 80–125% interval is not arbitrary - it is derived from population pharmacokinetic modeling, validated across thousands of real-world cases. The 0.8% seizure rate cited in JAMA? That’s statistically indistinguishable from baseline variability in epilepsy. To claim generics are unsafe is to misunderstand both statistics and pharmacology.
Liz MENDOZA
January 7, 2026 AT 02:25Will, thank you for saying that. I’ve had patients cry because they were told their generic was ‘just as good’ - but they felt different. We don’t dismiss them. We check the manufacturer, switch back if needed, and document everything. Science is great - but people come first.
Miriam Piro
January 7, 2026 AT 11:31They say bioequivalence is science - but who controls the data? The same companies that make the brand drugs. The generic manufacturers submit their own studies. No independent verification. The FDA is a revolving door. And don’t get me started on the ‘healthy volunteers’ - they’re all paid students who don’t have diabetes, heart disease, or depression. The real patients? They’re the lab rats. This isn’t medicine - it’s a controlled experiment on the poor.
Alex Lopez
January 9, 2026 AT 05:55Wow. So we’ve got a conspiracy theorist, a pseudo-philosopher, and a guy who thinks Ayurveda cures everything… all in one thread. Meanwhile, I’ve been prescribing generics since 2008. Zero lawsuits. Zero hospitalizations from bioequivalence failure. Just happy patients saving $300/month. The system works. If yours doesn’t? Talk to your doctor. Don’t blame the FDA because you watched a YouTube video titled ‘Big Pharma’s Secret.’ 😒