When you’re on antibiotics, your gut pays the price. Even if the medicine kills the bad bacteria, it doesn’t discriminate-it wipes out good ones too. That’s why so many people end up with bloating, diarrhea, or yeast infections while taking antibiotics. The good news? Probiotics can help. But only if you take them at the right time. Taking them together with your antibiotic? That’s like sending in reinforcements right before the battle starts. They won’t survive. The key isn’t just taking probiotics-it’s spacing them properly.
Why Timing Matters More Than You Think
Antibiotics work by killing bacteria. That’s their job. Probiotics are live bacteria. If you swallow them at the same time as your antibiotic, the antibiotic will kill the probiotic before it even has a chance to reach your gut. Studies show that when taken together, up to 92% of probiotic bacteria are destroyed. That means you’re wasting money and missing out on protection. The fix? Wait at least two hours between your antibiotic and your probiotic. This gives the antibiotic time to pass through your stomach and upper intestine without wiping out the helpful microbes. It’s not a guess-it’s backed by clinical trials. A 2013 study in the Journal of the American Medical Association showed that patients who spaced their probiotics by two hours had significantly lower rates of antibiotic-associated diarrhea (AAD). That’s diarrhea caused by antibiotics, not the infection itself.How Much Probiotic Do You Actually Need?
Not all probiotics are created equal. A cheap supplement with 1 billion CFUs (colony-forming units) won’t cut it. You need enough live bacteria to make a difference. Here’s what the science says:- Mild symptoms or short courses (3-5 days): 5-10 billion CFUs per day
- Diarrhea or moderate disruption: 10-20 billion CFUs per day
- Long courses (over 14 days) or existing gut issues: 20-40 billion CFUs per day
Which Probiotic Strains Actually Work?
There are hundreds of probiotic products on the shelf. But only a few strains have solid proof they help during antibiotic use.- Lactobacillus rhamnosus GG (LGG) - Best for preventing diarrhea in kids and adults. Proven in over 20 clinical trials.
- Saccharomyces boulardii CNCM I-745 - A yeast, not a bacteria. This one can be taken at the same time as antibiotics because antibiotics don’t kill yeast. It’s especially helpful for preventing Clostridium difficile infections.
- Bifidobacterium species - Good for restoring balance after antibiotics. Often paired with LGG in multi-strain formulas.
When to Start and How Long to Keep Going
Don’t wait until you feel sick. Start your probiotic as soon as you begin your antibiotic-ideally within 48 hours. A 2022 Cochrane Review found that people who started probiotics early reduced their risk of diarrhea by 71% compared to those who waited. And don’t stop when the antibiotics run out. Your gut needs time to recover. The standard recommendation? Keep taking probiotics for 7 to 14 days after your last antibiotic dose. One 2024 study showed that people who did this had 89% recovery of their gut microbiome. Those who stopped early? Only 63% recovered.What About Saccharomyces boulardii? Can You Take It With Antibiotics?
Yes. And this is important. Saccharomyces boulardii is a yeast. Antibiotics target bacteria, not fungi. That means you can take this probiotic at the same time as your antibiotic without losing effectiveness. It’s the only major probiotic that doesn’t need spacing. This makes it ideal for people on long-term antibiotics or those who struggle with timing. It’s also the most studied probiotic for preventing C. difficile infections-a serious, sometimes life-threatening condition that can follow antibiotic use.Real-Life Scheduling: How to Make It Stick
Most people fail not because the science is unclear, but because they forget. Here’s how to make it simple:If you take your antibiotic twice a day-at 8 a.m. and 8 p.m.-here’s your schedule:
- 6 a.m.: Probiotic
- 8 a.m.: Antibiotic
- 10 a.m.: Probiotic (if taking twice daily)
- 6 p.m.: Probiotic
- 8 p.m.: Antibiotic
- 10 p.m.: Probiotic (if taking twice daily)

What Happens If You Skip a Dose?
Missing one probiotic dose won’t ruin everything-but it does reduce effectiveness. A 2023 study tracking 217 people on antibiotics found that skipping just one day cut probiotic benefits by 37%. Consistency matters more than perfection. If you forget, take it as soon as you remember. Don’t double up. Just get back on track. And if you’re on a 14-day antibiotic course, plan ahead. Set phone reminders. Use a pill organizer. This isn’t optional-it’s the difference between mild discomfort and a full-blown gut crash.Common Mistakes to Avoid
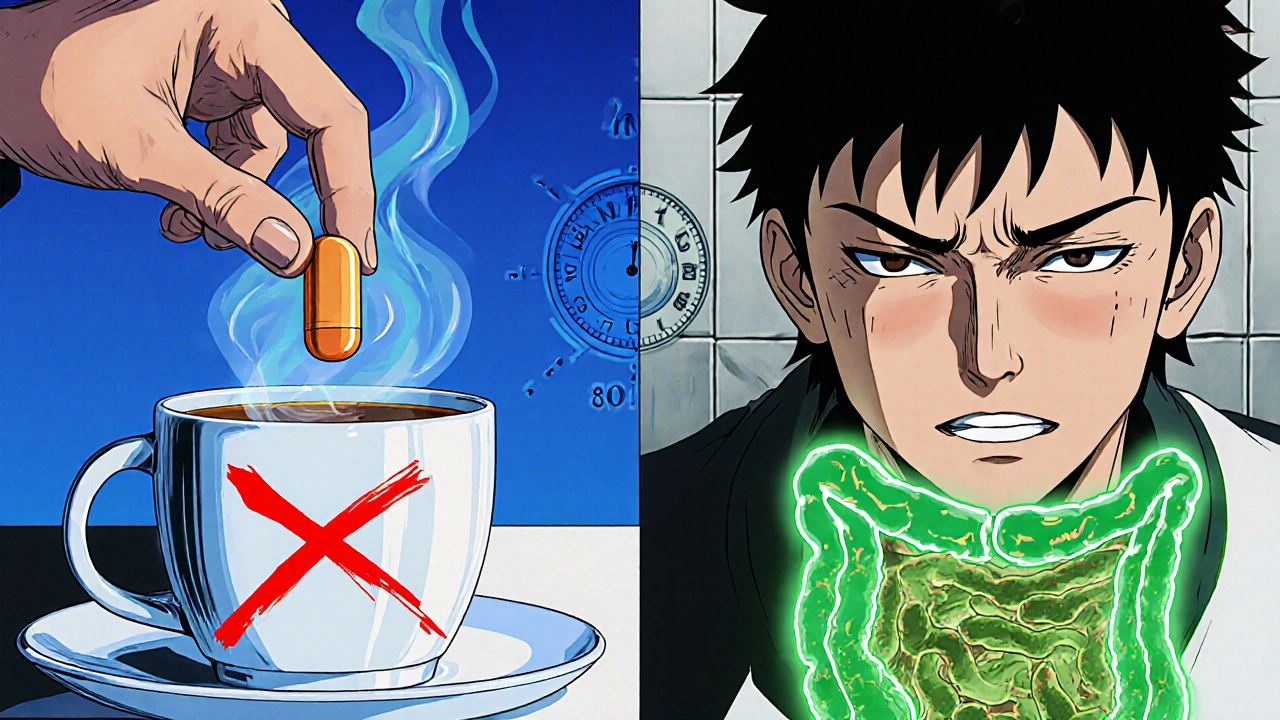
- Taking probiotics with food that’s too hot. Heat kills probiotics. Don’t mix them into hot coffee or soup.
- Choosing the cheapest option. Low-dose or unlabelled strains won’t help. Look for CFU count and strain names.
- Stopping too soon. Stopping when antibiotics end is the #1 mistake. Your gut needs extra time to rebuild.
- Assuming more strains = better. Studies show multi-strain formulas offer no advantage over single-strain ones for preventing AAD.
What’s Next? The Future of Probiotic Timing
Science is moving fast. Companies like Seed and Pendulum are now making time-release capsules that protect probiotics from stomach acid and antibiotics. Some are even testing smart formulations that release probiotics hours after the antibiotic passes through. Stanford University is running a $4.2 million study to see if we can one day personalize probiotic timing based on your unique gut microbiome. But right now, that’s still experimental. For now, the rules are clear: space your bacterial probiotics by two hours, use proven strains, take enough CFUs, and keep going for two weeks after your antibiotics. It’s simple. It’s science-backed. And it works.Can I take probiotics at the same time as antibiotics?
Only if you’re taking Saccharomyces boulardii, a yeast-based probiotic. Antibiotics don’t kill yeast, so it survives. For all bacterial probiotics like Lactobacillus or Bifidobacterium, you must wait at least two hours after your antibiotic dose. Taking them together kills up to 92% of the good bacteria before they can help.
How long should I keep taking probiotics after antibiotics?
Continue for 7 to 14 days after your last antibiotic dose. Your gut microbiome takes time to recover, and stopping too soon means you lose most of the benefit. Studies show people who kept taking probiotics for 14 days after antibiotics had nearly 30% better microbiome recovery than those who stopped early.
Do I need a high CFU count?
Yes. For most people on antibiotics, aim for at least 10 billion CFUs per day. If you’re on a long course or have had diarrhea before, go for 20-40 billion. Low-dose probiotics (under 5 billion) are unlikely to make a measurable difference in preventing side effects.
Are multi-strain probiotics better than single-strain ones?
No. Research shows no significant advantage. A single proven strain like Lactobacillus rhamnosus GG or Saccharomyces boulardii at the right dose works just as well-or better-than a mix of 10 weak strains. Don’t pay extra for marketing.
What if I forget to space them? Should I double the dose?
No. Doubling the dose won’t fix a missed window. Just take your next dose as scheduled. Consistency over time matters more than perfect timing every single day. Missing one dose reduces effectiveness by about 37%, but it doesn’t erase all progress.
Can I get probiotics from food instead of supplements?
Yogurt, kefir, sauerkraut, and kimchi contain probiotics, but they don’t provide the consistent, high doses needed during antibiotic treatment. A serving of yogurt might have 1-2 billion CFUs-far below the 10-40 billion recommended. Supplements are the only reliable way to get the right amount during antibiotic therapy.
Do probiotics interfere with the antibiotic’s ability to fight infection?
No. Multiple studies confirm that probiotics don’t reduce the effectiveness of antibiotics. In fact, they help you tolerate the treatment better, so you’re more likely to finish your full course. That’s critical-stopping antibiotics early leads to antibiotic resistance.
Is it safe to take probiotics while on strong antibiotics like vancomycin?
Yes. Vancomycin targets specific bacteria, and most probiotic strains still survive if spaced properly. Saccharomyces boulardii is especially safe with vancomycin since it’s not affected by antibiotics. Always stick to the two-hour rule unless your doctor says otherwise.




Scarlett Walker
November 14, 2025 AT 17:03Finally someone breaks this down without the fluff! I was taking probiotics with my antibiotics for months and wondered why I still got the runs. Two-hour gap? Game changer. Started last week and my gut’s been chill since. No more midnight bathroom dashes 😌
Anjan Patel
November 15, 2025 AT 22:55Oh PLEASE. You think it’s that simple? Everyone and their auntie is on probiotics now like it’s some magic potion. My cousin in Bangalore took 40 billion CFUs and still got C. diff. You’re just feeding the supplement industry. Real medicine doesn’t need fairy dust.
Ashley Durance
November 17, 2025 AT 18:48Let’s be real - the 92% stat is cherry-picked from one 2013 meta-analysis. Most of the probiotic research is low-quality, industry-funded, and underpowered. The Cochrane Review you cited? It says ‘may reduce risk’ - not ‘will prevent.’ Don’t confuse correlation with causation. You’re selling hope, not science.
Ryan Anderson
November 17, 2025 AT 20:54This is exactly the kind of info I wish my doctor had given me 🙏 I was on clindamycin for 10 days and ended up in a yeast infection spiral. Started LGG at 20B CFUs, spaced 2 hours out - and boom, zero issues. Also, Saccharomyces boulardii? Lifesaver. I now keep it in my medicine cabinet like oxygen. 🌿💪
Hrudananda Rath
November 18, 2025 AT 21:42One must question the intellectual integrity of this article. The reliance on CFU counts as a metric is a gross reductionism of microbiological ecology. The gut is not a petri dish. To prescribe dosages like pharmaceuticals is to misunderstand the very nature of symbiosis. The author reduces an intricate, co-evolved system to a spreadsheet. Shameful.
Nathan Hsu
November 20, 2025 AT 17:57Wait, wait, wait - you said Saccharomyces boulardii can be taken with antibiotics? Yes! I’ve been doing this for years - and yes, it’s a yeast, so antibiotics don’t touch it! But here’s the thing - I also take it with a spoonful of raw honey - helps it stick to the gut lining! And I only buy the ones from France - CNCM I-745 is the gold standard, folks! Don’t settle for less!
Kevin Wagner
November 21, 2025 AT 03:24Y’all are overcomplicating this. I’m not a scientist, but I’m a dad who’s seen his kid puke for a week after amoxicillin. We started LGG at 15B CFUs, spaced it like clockwork - and now? No more ‘antibiotic belly.’ My wife even started taking it prophylactically before her dental work. It’s not magic - it’s just smart. Do the thing. Don’t be lazy.
Dilip Patel
November 22, 2025 AT 21:35Probiotics are a western scam. In India we’ve been eating curd with meals since forever - no fancy supplements needed. Your gut knows what to do. You just need to eat real food. This article is just another way for Americans to sell you pills. We don’t need your 40 billion CFUs. We have lassi.
Scott Saleska
November 24, 2025 AT 06:44Hey, just wondering - if someone’s on vancomycin for C. diff, does spacing still matter? I’m asking because my uncle’s in the hospital right now and they’re giving him probiotics at the same time. I’m worried. Should I say something? Or is this one of those ‘trust the doctor’ things?
Eleanora Keene
November 24, 2025 AT 18:51Scott - YES, speak up! Your uncle should absolutely ask. Vancomycin is strong, and while Saccharomyces boulardii is safe, bacterial probiotics still need spacing. Tell him to ask his nurse for a 2-hour window. He’s not being annoying - he’s being a hero. And if they say no, ask for a pharmacist consult. You’re doing great.
gent wood
November 25, 2025 AT 17:22Thank you for this. I’ve been researching this for months after my own antibiotic ordeal. The strain specificity point is critical. Most people buy whatever’s on sale. I now only buy products that list the strain, CFU count, and expiration date. No proprietary blends. No vague claims. And yes - I keep a log. It’s not paranoia. It’s precision.
Joe Goodrow
November 26, 2025 AT 14:34Probiotics? We don’t need that in America. We have real medicine. Back in my day, we just drank buttermilk and toughed it out. Now everyone’s on supplements like they’re vitamins. This country’s gone soft. Take your antibiotics, stop complaining, and eat some yogurt if you’re bored.
Don Ablett
November 26, 2025 AT 23:22The cited studies are methodologically sound but lack longitudinal data. The microbiome recovery metric of 89% is based on fecal metagenomics at day 21 - but the functional restoration of metabolic pathways remains unquantified. Until we measure SCFA production and mucosal adhesion, we are observing correlation, not clinical efficacy