Boxed Warning Risk Calculator
Calculate Your Risk
Risk Calculation Results
Every year, the FDA updates its list of boxed warnings-the strongest safety alerts for prescription drugs. These aren’t just small print. They’re bold, black-bordered warnings that sit right at the top of a drug’s prescribing information, screaming: this could kill you if used wrong. In 2025, 47 new or revised boxed warnings were issued, up from 42 in 2024. That’s a 12% jump. And it’s not random. These changes reflect real, growing dangers we’re only now starting to understand.
What Exactly Is a Boxed Warning?
A boxed warning, sometimes called a black box warning, is the FDA’s highest-level safety alert. It’s not for minor side effects like headaches or nausea. It’s reserved for risks that are serious, life-threatening, and often preventable. Think: sudden heart failure, liver failure, fatal breathing problems, or birth defects. The FDA first started requiring these in the 1970s, but the rules tightened dramatically in the last decade. Today, over 400 prescription drugs in the U.S. carry one. That’s about 12% of all approved medications.These aren’t suggestions. They’re legal requirements. Drugmakers must include them if post-market data shows a clear link between the drug and a deadly outcome. And if they don’t update them fast enough? The FDA can fine them up to $250,000 per violation.
What Changed in 2025?
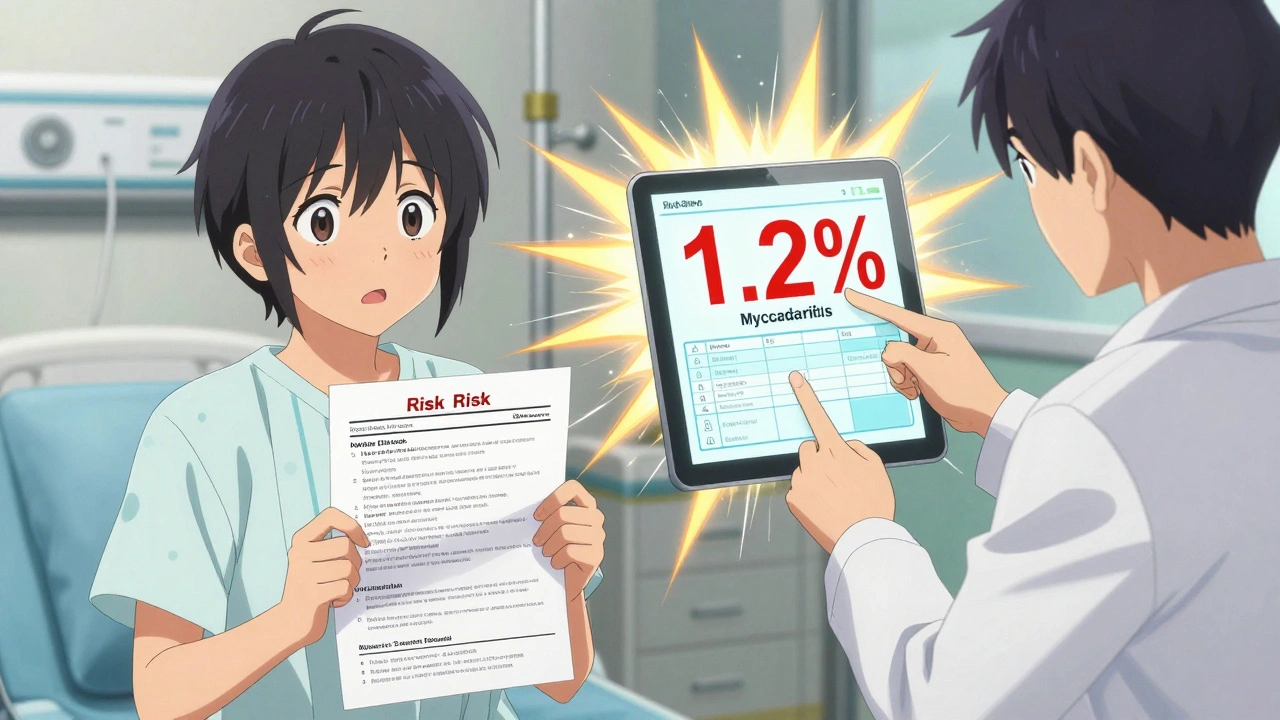
The 2025 updates weren’t just tweaks-they were major shifts. The biggest changes came in three areas: immunomodulators, GLP-1 agonists, and immune checkpoint inhibitors.For drugs like semaglutide (Ozempic, Wegovy) and tirzepatide (Mounjaro), new warnings now specify that myocarditis-heart inflammation-can occur in patients under 30, with an incidence rate of 1.2%. That’s not rare. It’s measurable. And it’s now required to be stated clearly in the warning, not buried in fine print.
Immunomodulators like dupilumab (Dupixent) and risankizumab (Skyrizi) got updated warnings for increased risk of serious infections, including tuberculosis reactivation. The new language doesn’t just say “monitor for infection.” It says: “Check TB status before starting. Repeat testing if patient has been exposed to TB or travels to high-risk areas.”
And for cancer drugs like pembrolizumab (Keytruda), the warning now includes a specific risk for immune-related colitis that can become fatal within 72 hours if untreated. The update requires oncologists to order stool tests and CRP levels within 48 hours of new diarrhea symptoms-not just “watch for side effects.”
These aren’t vague. They’re precise. That’s because the FDA’s 2023 Modernization Act now demands quantified risk data. No more “may cause liver damage.” Now it’s: “1.8% of patients under 50 develop ALT levels >3x upper limit of normal within 6 months.”
Why This Matters to Patients and Doctors
For patients, these changes mean better-informed choices. If you’re on a GLP-1 agonist and you’re 28, your doctor can now tell you: “There’s a 1 in 80 chance your heart could get inflamed. We’ll check your troponin if you get chest pain or extreme fatigue.” That’s not fearmongering. That’s transparency.For doctors, it’s a different story. Many say they’re overwhelmed. A 2024 Medscape survey found that 44% of physicians feel boxed warnings sometimes delay critical treatment-especially in emergencies. A doctor treating sepsis might hesitate to give moxifloxacin because of its QT prolongation warning, even though the patient’s EKG is normal. The alert is there. The system forces them to click through it. But is it helping-or just adding friction?
And here’s the real problem: not all warnings are created equal. A 2023 JAMA study found that only 43% of boxed warnings include specific, actionable steps. Some still say “monitor for hepatotoxicity.” But what does that mean? When? How often? The FDA’s 2025 update cracked down on that. Now, if a drug causes liver damage, the warning must say: “Check liver enzymes at baseline, week 2, week 4, and monthly for the first 6 months.” No more guessing.
How Hospitals Are Adapting
Hospitals aren’t ignoring this. The Joint Commission now requires triple-check systems for any drug with a boxed warning. At Henry Mayo Newhall Hospital, pharmacists must verify opioid tolerance before dispensing fentanyl patches. At Johns Hopkins, nurses use a checklist before giving methotrexate: “Is this weekly? Did we confirm renal function? Did the patient sign the safety agreement?”Electronic health records are changing too. New systems don’t just pop up a warning-they adjust the alert based on patient data. If you’re over 65 and on warfarin, the system flags you for bleeding risk. If you’re pregnant and on isotretinoin, it locks the prescription until you complete the iPledge program. That’s not automation. That’s intelligent safety.
But it’s not perfect. A Reddit thread from January 2025 showed that 61% of pharmacists said warfarin overrides happened because the EHR didn’t show the patient’s last INR. The system didn’t have the data. So the pharmacist guessed. That’s a failure of integration, not intent.

The Bigger Picture: Are Boxed Warnings Working?
Yes-and no.Since 2015, the FDA estimates these warnings have prevented 12,000 serious adverse events each year. That’s real. But they’re not foolproof. Rosiglitazone’s 2007 warning cut prescriptions by 70%. Pioglitazone got the same warning-and prescriptions barely budged. Why? Media coverage. Public fear. Perception matters as much as data.
And then there’s the “background noise” problem. NSAIDs have had a GI bleeding warning for decades. Most doctors don’t even read it anymore. That’s the danger of overuse. When every drug has a black box, they lose their power.
The solution? Precision. The FDA’s 2025 pilot program tested “dynamic” warnings that change based on age, kidney function, or prior history. In early trials, alert fatigue dropped 37%. That’s huge. If the system knows you’re 70 with stage 3 kidney disease, it shouldn’t show you the same warning it shows a healthy 30-year-old.
What You Should Do Now
If you’re a patient: Ask your doctor, “Does my medication have a boxed warning? What’s the real risk-and what do I need to watch for?” Don’t accept vague answers. Demand specifics.If you’re a clinician: Don’t just click through alerts. Read them. Update your protocols. Train your team. If you’re prescribing a new drug with a boxed warning, give your patient a printed summary. Make sure they understand the signs of trouble.
If you’re a pharmacist: Verify. Double-check. Don’t assume the EHR got it right. If the INR is missing, call the clinic. If the patient’s opioid tolerance isn’t documented, pause. Your judgment matters.
The bottom line? Boxed warnings aren’t about scaring people. They’re about saving lives. And in 2025, they’re getting smarter, sharper, and more personal. The question isn’t whether they matter. It’s whether we’re ready to use them right.
What drugs commonly have boxed warnings in 2025?
In 2025, the most common drugs with boxed warnings include GLP-1 agonists like semaglutide and tirzepatide (for myocarditis risk), immune checkpoint inhibitors like pembrolizumab (for fatal colitis), immunomodulators like dupilumab (for serious infections), and opioids like fentanyl patches (for respiratory depression in opioid-naïve patients). Warfarin, methotrexate, valproic acid, and clozapine also carry long-standing warnings for bleeding, liver toxicity, and agranulocytosis, respectively.
Can a boxed warning be removed?
Yes, but it’s rare. The FDA can remove a boxed warning if new data shows the risk is no longer significant or can be fully managed without the alert. For example, the warning for the antidepressant fluoxetine was reduced in 2020 after long-term studies showed suicidal ideation risk was limited to the first few weeks of treatment. Removal requires robust post-marketing evidence and usually takes years of data collection.
Do boxed warnings affect drug prices?
They often do. Drugs that receive a new boxed warning typically see a 20-25% drop in sales within a year, according to IMS Institute data. This is especially true for non-essential medications. But drugs with no alternatives-like warfarin or insulin-see little change in usage, even with strong warnings. The market responds to risk, but not always to fear.
Why do some doctors ignore boxed warnings?
Some doctors override warnings because they believe the risk is outweighed by benefit-especially in palliative care or emergency settings. Others cite poor EHR design: if the warning doesn’t give clear guidance or appears too often, it becomes noise. A 2024 Sermo survey found 73% of physicians routinely override warnings for dying patients, believing the theoretical risk is less urgent than symptom relief.
Are boxed warnings the same worldwide?
No. The U.S. FDA is the most aggressive in using boxed warnings. The European Medicines Agency (EMA) uses similar alerts but calls them “contraindications” or “special warnings.” Other countries often rely on general cautionary statements. A drug with a U.S. boxed warning might only have a standard caution in Canada or Australia. Always check local guidelines when prescribing or traveling with medication.




Jay Everett
December 2, 2025 AT 14:16Finally, someone’s talking about this like it matters. 🙌 The FDA’s 2025 updates are the first time in a decade I’ve seen real precision in these warnings-no more ‘monitor for hepatotoxicity’ nonsense. Now it’s ‘check LFTs at baseline, week 2, week 4, monthly.’ That’s not bureaucracy. That’s medicine catching up to reality. I’ve seen patients die because someone skipped the lab check. This isn’t fearmongering-it’s damage control with a pulse.
Zed theMartian
December 3, 2025 AT 02:08Oh wow. The FDA’s now playing doctor? Next they’ll be telling me how to breathe. You know what’s *really* dangerous? Trusting a government agency that can’t even get the date right on a press release to make life-or-death calls on drugs. This isn’t safety-it’s liability theater. I’ve seen 70-year-olds on warfarin with INRs of 1.8 get denied meds because some algorithm screamed ‘BLEEDING RISK’-even though the patient had been stable for 12 years. This isn’t progress. It’s digital panic.
Ella van Rij
December 3, 2025 AT 06:16sooooo… the FDA finally figured out that ‘monitor for liver damage’ isn’t a clinical instruction? 🤦♀️ i mean, congrats? took them 50 years. also, ‘check TB status before starting dupilumab’-did we just invent the concept of ‘do a basic test before giving a drug that suppresses immunity’? i’m crying. literally. my tears are made of bureaucratic irony.
ATUL BHARDWAJ
December 4, 2025 AT 09:22Boxed warnings are good. But in India, we don't have EHR. We don't have labs. We don't have time. Doctor sees patient. Gives pill. Patient goes home. Warning exists. But life is not a FDA manual.
Rebecca M.
December 5, 2025 AT 20:13Oh great. So now my doctor has to click through 17 pop-ups before prescribing me a pill that might save my life? And if he skips one? He gets sued? Meanwhile, my insurance denies my copay because the drug has a ‘black box’-even though I’ve been on it for 8 years and my heart is fine. This isn’t safety. It’s a lawsuit factory with a side of guilt.
Elizabeth Grace
December 6, 2025 AT 12:54my mom is on semaglutide. she’s 54. no heart issues. but now her doctor won’t refill it unless she gets an echo and a troponin test every 3 months. it’s $800. every 3 months. for a drug that helps her lose 2 lbs a week. i love that the FDA cares. but who’s paying for the emotional toll? the anxiety? the ‘what if’ nightmares? this isn’t transparency. it’s trauma with a prescription label.
Steve Enck
December 7, 2025 AT 01:51While the regulatory posture of the FDA in 2025 reflects a commendable ontological shift toward evidence-based risk stratification, the operational implementation remains plagued by systemic epistemological dissonance. The conflation of quantified incidence rates with clinical necessity introduces a performative dimension to clinical decision-making, wherein compliance supersedes contextual judgment. Furthermore, the institutionalization of algorithmic alerting mechanisms-while ostensibly reducing human error-has engendered a phenomenon of cognitive disengagement among prescribers, thereby paradoxically increasing the probability of adverse events through habitual override. The efficacy of boxed warnings, therefore, must be evaluated not as a binary of safety versus negligence, but as a complex adaptive system wherein sociotechnical friction dominates clinical outcomes.
dave nevogt
December 8, 2025 AT 22:36I’ve been a nurse for 22 years. I’ve seen people die from things that were never warned about. And I’ve seen people live because someone actually read the fine print. This isn’t about scaring people. It’s about giving them the truth before they sign the consent form. I remember a 26-year-old guy on Ozempic who came in with chest pain. He didn’t think it was serious. Said he was ‘just tired.’ His troponin was through the roof. Myocarditis. He almost didn’t make it. The new warning says ‘1 in 80.’ That’s not a number. That’s a kid. That’s a parent. That’s someone’s future. We used to say ‘watch for symptoms.’ Now we say ‘check this, do that, call if this happens.’ That’s not red tape. That’s love in a lab coat.
Joel Deang
December 9, 2025 AT 01:55so like… the FDA finally got smart? 😍 i mean, i used to think boxed warnings were just there to make docs feel guilty. but now they’re actually telling you what to DO? like ‘check INR’ not just ‘watch out’? that’s kinda beautiful. also, i typoed ‘INR’ as ‘INR’ 3 times while typing this. sorry. i’m tired. but this? this is good. 🙏
मनोज कुमार
December 9, 2025 AT 17:18Boxed warning is just marketing tool. Pharma companies pay FDA to add warnings to kill competitors. Semaglutide warning? Funny. Ozempic is now only drug for weight loss. Who benefits? Big Pharma. Not patients.
Roger Leiton
December 10, 2025 AT 20:50Can we just take a second to appreciate how far we’ve come? 🤯 I remember when the only warning on warfarin was ‘don’t eat kale.’ Now the system knows your age, your kidney function, your last INR, and if you’re pregnant-it even locks the script until you finish iPledge. It’s not perfect. But it’s trying. And that’s more than I can say for most tech these days. 🙏❤️